Sciatica
A common cause of back & leg pain
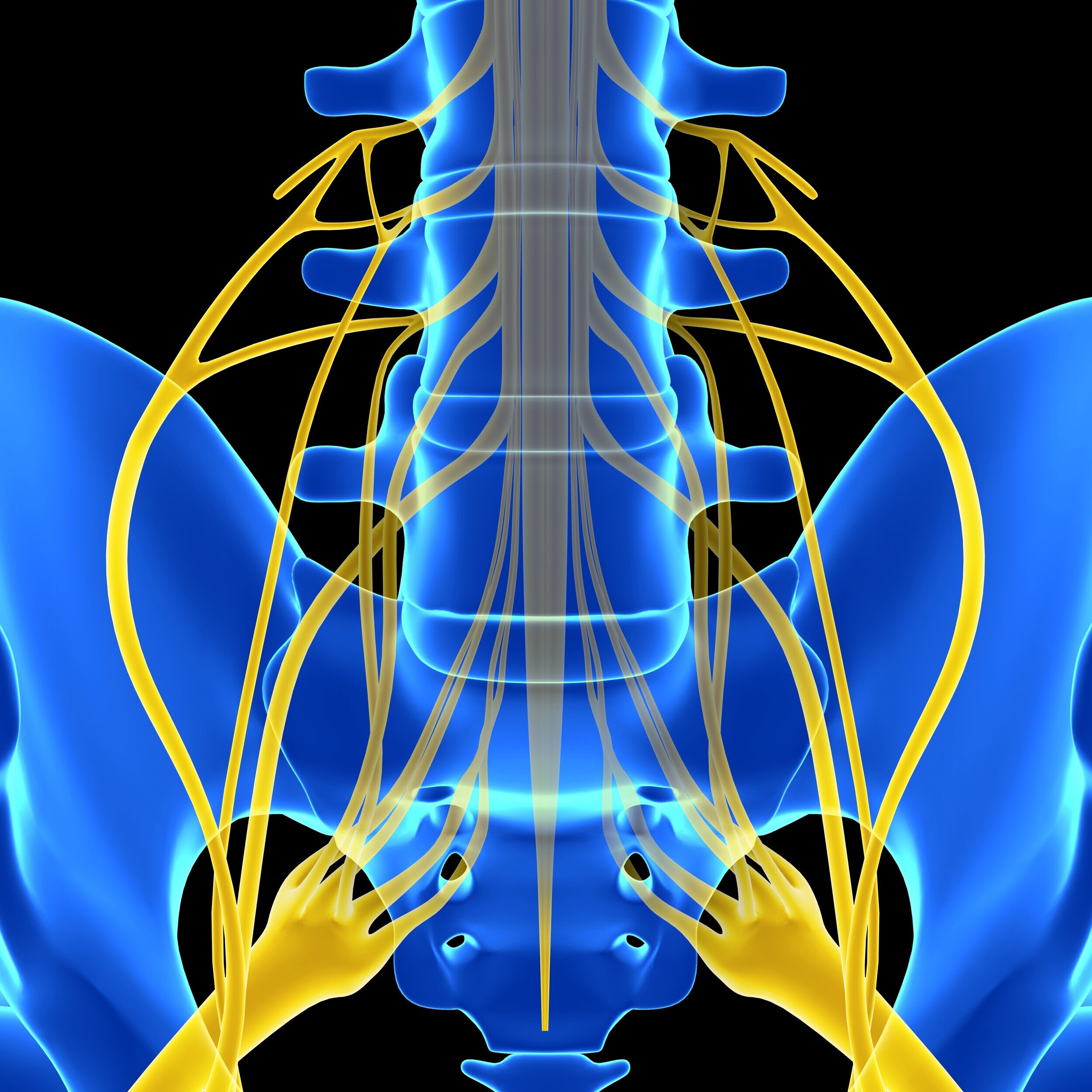
What Is Sciatic Nerve?
Sciatic nerve is the largest single nerve in the body, it starts in the lower spine & runs down the back of each leg. It controls the muscles of the back of the knee and lower leg. It also provides sensation to the back of the thigh, part of lower leg & the sole of the foot.
What is Sciatica?
Sciatica is a set of symptoms caused by general compression or irritation of one of nerve roots (L4 to S3) of sciatic nerve.
Symptoms include:
Lower back pain
Buttock pain, and numbness
Pain or weakness in various parts of the leg and foot.
"Pins and needles" sensation, or tingling in the leg
What are the common causes of Sciatica?
Spinal disc herniation
Herniated disc pressing on one of the lumbar or sacral nerve roots is the primary cause of sciatica, being present in about 90% of cases.
Spinal stenosis
This is a condition in which the spinal canal narrows and compresses the spinal cord or sciatic nerve roots. This narrowing decreases available space for the spinal cord, thus pinching and irritating nerves from the spinal cord that travel to the sciatic nerves.
Piriformis syndrome
In some people, the sciatic nerve runs through, or under the piriformis muscle. When the muscle shortens or spasms , it causes compression of the sciatic nerve. Piriformis syndrome can cause sciatica when the nerve root is normal.
Pregnancy
Spinal Tumors
Trauma to spine such as car accident
“I've been dealing with back pain for about a year and with the interventions Dr. Goswami and his medical team introduced to me, my pain has improved about 90%. I actually told him that I thought these intervention would never work, he made me a believer...”
— Craig Cochran
How do you treat sciatica?
Conservative treatment
Applying heat or ice to the painful area
Taking over the counter pain relievers such as Tylenol or Ibuprofen
Physical Therapy
Medical management
Certain medication such as anticonvulsants and antidepressants are known to benefit patients suffering from sciatica.
Minimally Invasive Treatment
Open Surgery
Usually reserved for very few patients with pain from structural anatomical problems that have not responded to medical or interventional therapy.
What is Epidural Steroid Injection?
Epidural Steroid Injection is a technique for relieving pain from disc herniation. A small amount of corticosteroid is injected into the epidural space around the spinal cord and spinal nerves. The anti-inflammatory effects of the corticosteroid is responsible for providing pain relief.
What is Endoscopic Discectomy?
Endoscopic Discectomy is a procedure used to remove damaged disc material in the spine. It is a minimally invasive technique that unlike the conventional procedure does not involve major tissue injury.

